The Right Way To Prevent Posterior Calcaneal Spur

Overview
Although a heel spur is often thought to be the source of heel pain, it rarely is. When a patient has plantar fasciitis, the plantar fascia pulls on the bottom of the heel bone. Over time this can cause a spur to form. Heels spurs are a very common x-ray finding, and because the heel spur is buried deep in soft tissue and not truly in a weight bearing area, there is often no history of pain. It is important to note that less than one percent of all heel pain is due to a spur. but frequently caused by the plantar fascia pulling on the heel. Once the plantar fasciitis is properly treated, the heel spur could be a distant memory.
Causes
Bone spurs can form anywhere in the feet in response to tight ligaments, repetitive stress injuries (typically from sports), obesity, even poorly fitting shoes. For instance, when the plantar fascia on the bottom of the foot pulls repeatedly on the heel, the ligament becomes inflamed, causing plantar fasciitis. As the bone tries to mend itself, a bone spur forms on the bottom of the heel, typically referred to as a heel spur. This is a common source of heel pain.

Symptoms
With heel spurs, people often talk about a dull ache which is felt most of the time with episodes of a sharp pain in the center of the heel or on the inside margin of the heel. Often the pain is worse on first rising in the morning and after rest and is aggravated by prolonged weight bearing and thin-soled shoes.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
Over-the-counter or prescription-strength anti-inflammatory medications can help temporarily, but can cause side effects with prolonged use - the most significant being gastrointestinal upset, ulceration and bleeding. Deep tissue massage, taping and other physical therapy modalities can also be helpful. Arch support is highly recommended, either with shoe inserts or custom orthotics made by podiatrists. If pain continues, a steroid injection at the site of pain may be recommended; however, many physicians do not like injecting around the heel. The side effects of steroids injected in this area can be serious and worsen symptoms. Complications can include fat necrosis (death of fatty tissue) of the heel and rupture of the plantar fascia.
Surgical Treatment
Though conservative treatments for heel spurs work most of the time, there are some cases where we need to take your treatment to the next level. Luckily, with today?s technologies, you can still often avoid surgery. Some of the advanced technologies to treat a Heel Spur are Platelet Rich Plasma Therapy. Platelet Rich Plasma Therapy (also known as PRP) is one of several regenerative medicine techniques that University Foot and Ankle Institute has helped bring to foot and ankle care. This amazing in-office procedure allows the growth factors in the blood to be used to actually begin the healing process again long after your body has given up on healing the area. Heel Pain Shockwave Therapy. Shockwave therapy is a non-invasive procedure done in the office that allows for new blood to get to the region of fascia damage and help with healing. Results have been excellent with more than 70 percent of patients getting relief with only one treatment. Topaz for Heal Spurs and pain. Another minimally invasive technology technique is called Coblation Surgery using a Topaz probe. This minimally invasive procedure involves controlled heating of multiple tiny needles that are inserted through the skin and into the plantar fascia. This process, like PRP and Shockwave therapy, irritates the fascia enough to turn a chronic problem back into an acute problem, greatly increasing the chances of healing. Heel Spur Surgery. Endoscopic Plantar Fasciotomy is one surgical procedure that we consider to release the tight fascia. University Foot and Ankle Institute has perfected an endoscopic (camera guided) approach for fascia release to allow rapid healing and limited downtime with minimal pain.
Prevention
Walk around before you buy shoes. Before you purchase your shoes, do the following. Re-lace the shoes if you're trying on athletic shoes. Start at the farthest eyelets and apply even pressure to the laces as you come closer to the tongue of the shoe. Make sure that you can wiggle your toes freely inside of the shoe. Also, make sure that you have at enough space between your tallest toe and the end of the shoe. You should have room equal to about the width of your thumb in the tip of your shoe. Walk around to make sure that the shoe has a firm grip on your heel without sliding up and down. Walk or run a few steps to make sure your shoes are comfortable. Shoes that fit properly require no break-in period.
Bursitis Feet Pads
Between the heel bone and the plantar fascia is a small fluid filled sac that is called the plantar (bottom of) calcaneal (heel bone) bursa. The plantar calcaneal bursa?s job is to allow the plantar fascia to glide easily over the heel bone without irritation. If this becomes inflamed and irritated a plantar calcaneal bursitis occurs which can be extremely painful and disabling forcing the athlete to stop training.
Causes
A bursa is a fluid-filled sac that acts as a cushion and a lubricant between tendons and muscles sliding over bone. There are bursas around most large joints in the body, including the ankle. The retrocalcaneal bursa is located in the back of the ankle by the heel, where the large Achilles tendon connects the calf muscles to the heel bone (calcaneus). Repetitive or over use of the ankle, for instance by doing excessive walking, running or jumping, can cause this bursa to become irritated and inflamed. This condition is commonly associated with Achilles tendonitis. Sometimes retrocalcaneal bursitis may be mistaken for achilles tendonitis. Those at risk for this condition include people just starting aggressive exercise regimens or having some other sudden increase in activity without proper conditioning.
Symptoms
Symptoms of Achilles bursitis are often mistaken for Achilles tendinitis because of the location of the pain at the back of the heel. When you suffer from Achilles bursitis you will experience some or all of the following symptoms which are most noticeable when you begin activity after resting. High heels can add pressure on the retrocalcaneal bursa, subcutaneous calcaneal bursa, and Achilles tendon.
Diagnosis
During the physical examination of a patient with calcaneal bursitis, the physician should keep the following considerations in mind. Swelling and redness of the posterior heel (the pump bump) may be clearly apparent. The inflamed area, which may be slightly warm to the touch, is generally tender to palpation. Careful examination can help the clinician to distinguish whether the inflammation is posterior to the Achilles tendon (within the subcutaneous calcaneal bursa) or anterior to the tendon (within the subtendinous calcaneal bursa). Differentiating Achilles tendinitis/tendinosis from bursitis may be impossible. At times, the 2 conditions co-exist. Isolated subtendinous calcaneal bursitis is characterized by tenderness that is best isolated by palpating just anterior to the medial and lateral edges of the distal Achilles tendon. Conversely, insertional Achilles tendinitis is notable for tenderness that is located slightly more distally, where the Achilles tendon inserts on the posterior calcaneus. A patient with plantar fasciitis has tenderness along the posterior aspect of the sole, but he/she should not have tenderness with palpation of the posterior heel or ankle. A patient with a complete avulsion or rupture of the Achilles tendon demonstrates a palpable defect in the tendon, weakness in plantarflexion, and a positive Thompson test on physical examination. During the Thompson test, the examiner squeezes the calf. The test is negative if this maneuver results in passive plantarflexion of the ankle, which would indicate that the Achilles tendon is at least partially intact.
Non Surgical Treatment
Treatments should involve decreasing swelling, relieving pain and stress on the Achilles, correcting any biomechanical dysfunction (over-pronation or flat feet), treating scar tissue, and then restoring strength and movement. If you are performing an activity that could cause further trauma to the bursa, it is recommended that you protect the area with padding and/or proper footwear to prevent further irritation or damage.
Surgical Treatment
Surgery is rarely need to treat most of these conditions. A patient with a soft tissue rheumatic syndrome may need surgery, however, if problems persist and other treatment methods do not help symptoms.
Prevention
Because many soft tissue conditions are caused by overuse, the best treatment is prevention. It is important to avoid or modify the activities that cause problems. Underlying conditions such as leg length differences, improper position or poor technique in sports or work must be corrected. Be aware of potential overuse or injury in your daily activities and change your lifestyle to prevent problems. Otherwise, problems may persist or occur repeatedly. Following are some ways you can avoid future problems. Wear walking or jogging shoes that provide good support. High-top shoes provide support for people with ankle problems. Wear comfortable shoes that fit properly. Wear heel cups or other shoe inserts as recommended by your doctor. Exercise on level, graded surfaces.
Can Hammertoes Cause Numbness
hammertoe most commonly affects the second toe on the foot. It Hammer toes causes the middle joint to bend. Hammertoe is most frequently caused by structural problems in the toe or from wearing poor fitting shoes. It is important to diagnose and treat hammertoe early because the condition tends to become worse over time. If left untreated, hammertoe can require surgery.
Causes
As described above, the main reason people develop hammertoes is improper footwear, or footwear that is too short for the toes. Shoes that do not allow our toes to lie flat are the biggest cause of hammertoes, though there are others, including genetics, injury or trauma in which the toe is jammed or broken. Diseases that affect the nerves and muscles, such as arthritis. Abnormal foot mechanics due to nerve or muscle damage, causing an imbalance of the flexor and extensor tendons of the toe. Systematic diseases such as arthritis can also lead to problems such as hammertoe. Some people are born with hammertoes, while others are more prone to developing the condition due to genetics. If you have ever broken a toe, you know there is not much that can be done for it. It is one of the only bones in the body that heals without the use of a cast. A broken toe may be splinted, however, which may help prevent a hammertoe from forming.
 Symptoms
Symptoms
The most common symptoms of hammertoes include. The toe is bent upward at the middle toe joint, so that the top of this joint rubs against the top of the shoe. The remainder of the toe is bent downward. Pain upon pressure at the top of the bent toe from footwear. The formation of corns on the top of the joint. Redness and swelling at the joint contracture. Restricted or painful motion of the toe joint. Pain in the ball of the foot at the base of the affected toe. This occurs because the contracted digit puts pressure on the metatarsal head creating callouse and pressure on the ball of the foot.
Diagnosis
Hammertoes are progressive, they don?t go away by themselves and usually they will get worse over time. However, not all cases are alike, some hammertoes progress more rapidly than others. Once your foot and ankle surgeon has evaluated your hammertoes, a treatment plan can be developed that is suited to your needs.
Non Surgical Treatment
Apply a commercial, nonmedicated hammertoe pad around the bony prominence of the hammertoe. This will decrease pressure on the area. Wear a shoe with a deep toe box. If the hammertoe becomes inflamed and painful, apply ice packs several times a day to reduce swelling. Avoid heels more than two inches tall. A loose-fitting pair of shoes can also help protect the foot while reducing pressure on the affected toe, making walking a little easier until a visit to your podiatrist can be arranged. It is important to remember that, while this treatment will make the hammertoe feel better, it does not cure the condition. A trip to the podiatric physician?s office will be necessary to repair the toe to allow for normal foot function. Avoid wearing shoes that are too tight or narrow. Children should have their shoes properly fitted on a regular basis, as their feet can often outgrow their shoes rapidly. See your podiatric physician if pain persists.
Surgical Treatment
If you have a severe case of hammer toe or if the affected toe is no longer flexible, you may need surgery to straighten your toe joint. Surgery requires only a local anesthetic (numbing medicine for the affected area) and is usually an outpatient procedure. This means you don?t have to stay in the hospital for the surgery.
Could Hammer Toes Trigger Leg Ache
 Overview
Overview
hammertoes is the general term used to describe an abnormal contraction or "buckling" of the toe because of a partial or complete dislocation of one of the joints of the toe or the joint where the toe joins with the rest of the foot. As the toe becomes deformed, it rubs against the shoe and the irritation causes the body to build up more and thicker skin to help protect the area. The common name for the thicker skin is a corn.
Causes
The most common cause of hammertoe is a muscle/tendon imbalance. This imbalance, which leads to a bending of the toe, results from mechanical (structural) changes in the foot that occur over time in some people. Hammertoes may be aggravated by shoes that don?t fit properly. A hammertoe may result if a toe is too long and is forced into a cramped position when a tight shoe is worn. Occasionally, hammertoe is the result of an earlier trauma to the toe. In some people, hammertoes are inherited.
 Symptoms
Symptoms
People with a hammer toe will often find that a corn or callus will develop on the top of the toe, where it rubs against the top of the footwear. This can be painful when pressure is applied or when anything rubs on it. The affected joint may also be painful and appear swollen.
Diagnosis
First push up on the bottom of the metatarsal head associated with the affected toe and see if the toe straightens out. If it does, then an orthotic could correct the problem, usually with a metatarsal pad. If the toe does not straighten out when the metatarsal head is pushed up, then that indicates that contracture in the capsule and ligaments (capsule contracts because the joint was in the wrong position for too long) of the MTP joint has set in and surgery is required. Orthotics are generally required post-surgically.
Non Surgical Treatment
People with a hammer toe benefit from wearing shoes in which the toe box is made of a flexible material and is wide enough and high enough to provide adequate room for the toes. High-heeled shoes should be avoided, because they tend to force the toes into a narrow, flat toe box. A doctor may recommend an insert (orthotic) for the shoe to help reduce friction and pressure on the hammer toe. Wearing properly fitted shoes may hammertoe reduce pain and inflammation. It may also prevent ulcers from developing and help existing ulcers heal. However, the hammer toe does not disappear.
Surgical Treatment
Sometimes, if the deformity is severe enough or surgical modification is needed, the toe bones may be fused so that the toe does not bend. Buried wires are used to allow for the fusion to heal, and they remain in place after healing. Your skin is closed with fine sutures, which are typically removed seven to ten days after surgery. A dressing is used to help keep your toes in their new position. Dressings should not get wet or be removed. After surgery, your doctor may prescribe pain relievers, typically for the initial four to seven days. Most people heal completely within one month of surgery, with few complications, if any. Crutches or a cane may be needed to help you keep weight off your affected foot, depending on the procedure. Occasionally, patients receive a special post-op shoe or a walking boot that is to be worn during the healing process. Most people are able to shower normally after surgery, but must protect the dressing from getting wet. Many patients are allowed to resume driving within one week after the procedure, but care needs to be taken.
Bilateral Hallux Valgus Deformity
Overview
 A bunion is generally considered as an enlargement of the joint (a lump of bone) at the base and side of the big toe (specifically, the first metatarsophalangeal joint). Bunions form when the toe moves out of place. As the big toe bends towards the others this lump becomes larger and the bunion can become painful, arthritis and stiffness can eventually develop. Hallux valgus or hallux abducto valgus (HAV) is the name used for the deviated position of the big toe and a bunion refers to the enlargement of the joint, most of the time the two go together and can just be referred to as 'bunions'. The word bunion is from the Latin "bunion," meaning enlargement.
A bunion is generally considered as an enlargement of the joint (a lump of bone) at the base and side of the big toe (specifically, the first metatarsophalangeal joint). Bunions form when the toe moves out of place. As the big toe bends towards the others this lump becomes larger and the bunion can become painful, arthritis and stiffness can eventually develop. Hallux valgus or hallux abducto valgus (HAV) is the name used for the deviated position of the big toe and a bunion refers to the enlargement of the joint, most of the time the two go together and can just be referred to as 'bunions'. The word bunion is from the Latin "bunion," meaning enlargement.
Causes
Women traditionally have a higher rate of bunions, which is to be expected, since it is they who have traditionally worn shoes with high heels, a narrow toe box, or whatever fashion dictates from year to year. However, men can suffer from bunions as well, as can anyone for whom the right (or wrong) conditions exist, poor foot mechanics, improper footwear, occupational hazards, health and genetic predisposition. Finally, bunions have long been a condition associated with the elderly, and although they often appear in conjunction with inflammatory joint diseases such as arthritis (which is often associated with age), they can strike at any point in life, including adolescence.
Symptoms
The most obvious symptoms of a bunion are. Pain in the area of the MTP joint, the joint where your big toe connects to your foot. Bending of the big toe in towards the other toes. An enlarged bump of bone or tissue at the MTP joint. Each symptom can range in degree from small to severe. Sometimes the pain can be sufficient to make it difficult to walk in normal shoes. Other symptoms may include. Swelling and inflammation of the skin around the MTP joint. Thickening of the skin in the area of the joint. Restricted motion in your big toe. Pressure from the inward bending of your big toe can affect your other toes, leading to corns on your smaller toes. Ingrown toenails on the smaller toes. Development of hammertoes in the other toes. Calluses on the bottom of your foot. If you have any of these symptoms, especially pain, displacement of your big toe or development of a bulge, you should consider consulting your physician. Even if you're not significantly bothered by some of these symptoms, bunions tend to continue getting bigger and more serious over time and should be taken care of before they do so.
Diagnosis
A doctor can very often diagnose a bunion by looking at it. A foot x-ray can show an abnormal angle between the big toe and the foot. In some cases, arthritis may also be seen.
Non Surgical Treatment
Wear comfortable shoes that don't squeeze your toes together. Sandals are ideal in warm weather. Cushioning the bunion with a donut-shaped bunion pad sold at drugstores can prevent any direct rubbing against your shoes. Have your shoes stretched to give your foot more room or consider switching to footwear customized to relieve pressure on the affected area. Soak your foot in warm water to help lessen the pain after a day on your feet. Apply ice packs several times a day to reduce swelling of painful and inflamed bunions. Take aspirin or ibuprofen for the inflammation and pain, and try supplementing with anti-inflammatory herbs such as ginger and turmeric (these work more slowly than the drugs). See a podiatrist for specially fitted shoes or orthotic devices that may help. Sometimes, surgery is necessary. Seek a second opinion before scheduling any operation. 
Surgical Treatment
Surgery might be recommended if non-surgical treatments fail to provide relief, and you are having trouble walking or are in extreme pain. Surgery can be used to return the big toe to its correct anatomical position. During surgery, bones, ligaments, tendons, and nerves are put back into correct order, and the bump is removed. Many bunion correction procedures can be done on a same-day basis. The type of procedure will depend on your physical health, the extent of the foot deformity, your age, and your activity level. The recovery time will depend on which procedure or procedures are performed. Surgery may be recommended to correct a tailor?s bunion, but is unlikely to be recommended for an adolescent bunion.
Overpronation Of The Feet Painfulness
Over Pronation (Flat Feet) refers to the biomechanical shock-absorbing motion of the ankle, foot and lower leg. It is the natural inward flexing motion of the lower leg and ankle. Standing, walking, and running cause the ankle joint to pronate which in turn helps the body to absorb shock and allows it to control balance. An ankle joint that is too flexible causes more pronation than desired. This common condition is called Over- Pronation (sometimes referred to as "Flat Feet"). This foot condition places an extreme degree of strain on various connective tissues of the ankle, foot, and knee. If this condition is not addressed foot pain and toe deformities such as bunions and hammer toes (just to name a couple) may develop. Hip and lower back pain may also be residual results from this condition.
Causes
A common cause of pronation is heredity - we can inherit this biomechanical defect. The second most common cause is due to the way our feet were positioned in the uterus while we were developing; this is called a congenital defect. In either instance, the following occurs in our feet during our development.
Symptoms
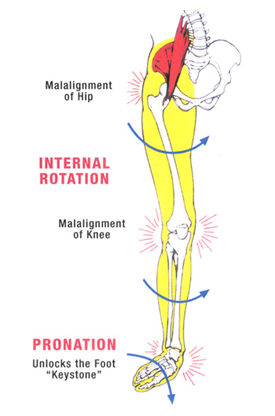
Overpronation can negatively affect overall body alignment. The lowering of the longitudinal arch pulls the heel bone in, causing the leg, thigh bone and hip to rotate inwards, and an anterior tilt of the pelvis. Unnecessary strain to the ankles, knees, hips and back can result. Plantar fasciitis and inflammation, metatarsal pain, problems with the Achilles tendon, pain on the inside of the knee, and bursitis in the hip are just some of the conditions commonly associated with pronation.
Diagnosis
Firstly, look at your feet in standing, have you got a clear arch on the inside of the foot? If there is not an arch and the innermost part of the sole touches the floor, then your feet are over-pronated. Secondly, look at your running shoes. If they are worn on the inside of the sole in particular, then pronation may be a problem for you. Thirdly, try the wet foot test. Wet your feet and walk along a section of paving and look at the footprints you leave. A normal foot will leave a print of the heel, connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot, shown opposite. The best way to determine if you over pronate is to visit a podiatrist or similar who can do a full gait analysis on a treadmill or using forceplates measuring exactly the forces and angles of the foot whilst running. It is not only the amount of over pronation which is important but the timing of it during the gait cycle as well that needs to be assessed.

Non Surgical Treatment
Supportive orthotics in the shoe is a method commonly implemented to treat many common running injuries associated with pronation. An advantage of orthotics is that they often allow the sufferer to continue to participate in athletic activity and avoid other treatment options that could be potentially costly and time consuming. Seventy-five percent of injured runners are successfully treated with the prescription of orthoses. Orthotics are the most effective treatment for symptoms that develop from unusual biomechanics within the body such as overpronation, resulting in either great improvement or complete healing of the injury in about half the cases.
Prevention
Firstly, a thorough and correct warm up will help to prepare the muscles and tendons for any activity or sport. Without a proper warm up the muscles and tendons around your feet, ankles and lower legs will be tight and stiff. There will be limited blood flow to the lower legs, which will result in a lack of oxygen and nutrients for those muscles. Click here for a detailed explanation of how, why and when to perform your warm up. Secondly, flexible muscles are extremely important in the prevention of most ankle and lower leg injuries. When muscles and tendons are flexible and supple, they are able to move and perform without being over stretched. If however, your muscles and tendons are tight and stiff, it is quite easy for those muscles and tendons to be pushed beyond their natural range of motion. To keep your muscles and tendons flexible and supple, it is important to undertake a structured stretching routine.
Coping With Calcaneal Apophysitis
Sever?s disease (also known as calcaneal apophysitis) is a type of bone injury in which the growth plate in the lower back of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and causes pain. Sever?s disease is the most common cause of heel pain in children, especially those who exercise or play sports on a regular basis.
Causes
Severs disease is caused by repetitive excessive force to the growing area of the heel bone, causing injury to this area. The calf muscles (soleus and gastrocnemius) are attached by the Achilles tendon to the calcaneus (heel bone). They exert a huge force during running , jumping and landing. In children, there is a growing area in the heel bone called the apophysis and is made of relatively weak cartilage. If there is excessive force at this relatively weak point damage occurs. This excess force can be caused by a number of factors. During the adolescent growth spurt the bones grow very quickly. The muscles do not grow out at the same rate as the bone grows and so can become very tight. The calf muscles generate huge forces when they are used to run, jump and land. This force is transmitted to the calcaneal apophysis (growth area). The gastrocnemius muscle spans both the ankle and knee joint. Tightness of this or any other muscles of the lower limb (hamstring or quadriceps) cause extra force at the growing (weak) area. In active children, who undertake a lot of exercise, the repetitive high force causes damage. If your child has poor biomechanics due to poor lower limb alignment (often caused by flat feet), the muscles of the lower limb have to work excessively hard and this can cause increased force at the tibial tubercle.
Symptoms
Sever?s disease is a clinical diagnosis based on the youth?s presenting symptoms, rather than on diagnostic tests. While x-rays may be ordered in the process of diagnosing the disease, they are used primarily to rule out bone fractures or other bone abnormalities, rather than to confirm the disease. Common Characteristics of Sever?s Disease include Posterior inferior heel pain. Pain is usually absent when waking in the morning. Increased pain with weight bearing, running, or jumping (or activity-related pain). Area often feels stiff or inflexible. Youth may limp at the end of physical activity. Tenderness at the insertion of the tendons. Limited ankle dorsiflexion range that is secondary to tightness of the Achilles tendon. Activity or sport practices on hard surfaces can also contribute to pain, as well as poor quality shoes, worn out shoes, or the wrong shoes for the sport. Typically, the pain from this disease gradually resolves with rest.
Diagnosis
A doctor can usually tell that a child has Sever's disease based on the symptoms reported. To confirm the diagnosis, the doctor will probably examine the heels and ask about the child's activity level and participation in sports. The doctor might also use the squeeze test, squeezing the back part of the heel from both sides at the same time to see if doing so causes pain. The doctor might also ask the child to stand on tiptoes to see if that position causes pain. Although imaging tests such as X-rays generally are not that helpful in diagnosing Sever's disease, some doctors order them to rule out other problems, such as fractures. Sever's disease cannot be seen on an X-ray.
Non Surgical Treatment
stretching exercises can help. It is important that your child performs exercises to stretch the hamstring and calf muscles, and the tendons on the back of the leg. The child should do these stretches 2 or 3 times a day. Each stretch should be held for about 20 seconds. Both legs should be stretched, even if the pain is only in 1 heel. Your child also needs to do exercises to strengthen the muscles on the front of the shin. To do this, your child should sit on the floor, keeping his or her hurt leg straight. One end of a bungee cord or piece of rubber tubing is hooked around a table leg. The other end is hitched around the child's toes. The child then scoots back just far enough to stretch the cord. Next, the child slowly bends the foot toward his or her body. When the child cannot bend the foot any closer, he or she slowly points the foot in the opposite direction (toward the table). This exercise (15 repetitions of "foot curling") should be done about 3 times. The child should do this exercise routine a few times daily.